Isokinetic Knee Extensor Testing Following ACL Reconstruction
Contents
• Preamble: Isokinetic Knee Extensor Testing Following ACL Reconstruction
• Positioning for Testing the Knee Extensors
• Anatomical Referencing
• Gravity Correction
• Range of Movement
• Warm-up
• Pre-loading the Isokinetic Movement
• Selecting Maximal Isokinetic Efforts
• Which and How Many Velocities?
• Quantitative Measures of Strength
• References
Preamble: Isokinetic Knee Extensor Testing Following ACL Reconstruction
It is recommended that you peruse the tutorial on Kin-Com Isokinetic Knee Testing (link to this tut) prior to this tutorial. The following tutorial recommends changes to the basic isokinetic knee extensor testing protocol when testing subjects post anterior cruciate ligament (ACL) reconstruction. These changes are based on a need to locate the resistance pad proximally on the tibia. This proximal pad placement has the effect of increasing the contact force between the leg and the pad, and it is this increased pad force which acts to assist the ACL in reducing and usually preventing an anterior shift of tibia on the femur. A preliminary reference to this work is referenced at the end of this tutorial.
An implication of the proximal pad placement is that the preload or initiating forces will be increased (in proportion to the increase in resistance pad forces). The discrete testing approach previously described (insert link to first tutorial here) is used. It typically consists of three to five (or more) maximal concentric and three to five (or more) maximal eccentric muscle actions per velocity, with each muscle action separated by a thirty second recovery time. A two minute recovery time is interspersed between each angular velocity of movement. At this time we are investigating the incorporation of three angular velocities for concentric muscle actions (60, 120 and 180 deg/s) and an angular velocity of 60 deg/s for maximal eccentric muscle actions. This testing is being conducted at 12, 18 and 24 weeks post ACL reconstructive surgery.
Positioning for Testing the Knee Extensors
The knee extensor protocol which incorporats both concentric and eccentric muscle actions can use either our standard neutral hip position (supine lying) or a hip flexed position (sitting). The supine lying position would be used when both knee extensor and knee flexor strength assessments are to be performed.
Both the supine lying and sitting positions have the knee joint protruding over the end of the Kin-Com bench. The thigh needs to be well supported, and the leg also must be able to achieve at least 90 degrees of knee flexion without the posterior aspect of the leg contacting the front edge of the bench. Check this position ensuring a space of two to three finger widths between the freely hanging leg and the front of the Kin-Com bench. This space is illustrated in the figure below.
Figure 1.
To stabilise the pelvis in the supine lying position, two straps are placed over the ASIS and slightly more distal. The subject either places their hands under their head or folds their arms across their chest. They are not allowed to grip the sides of the bench. In the sitting position one or two straps are placed around the subject’s pelvis. A thigh strap may be used but since the knee extensors alone are being tested (concentricaly and eccentrically) the thigh segment and the knee joint are very stable during maximal efforts.
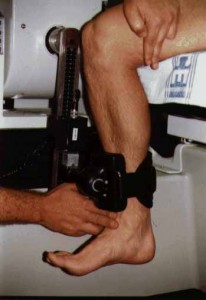
The knee joint centre (lateral femoral condyle) is aligned with the axis of rotation of the dynamometer by moving the Kin-Com bench. The resistance pad is located proximally on the leg at a distance from the knee joint axis of rotation of approximately 40% of leg length (measured from the lateral femoral condyle to the lateral malleolus). It is important that the centre of the resistance pad is aligned with a whole centimetre value on the lever arm ruler – this number is then the lever arm length.
Check the alignment of the knee joint centre by passively moving the leg through the full range of motion. If correctly aligned, the resistance pad should not tilt or slide along the leg.
For our most recent testing, we have modified a resistance pad from the Kin-Com AP to fit the Kin-Com 500H used in the Exercise Science Laboratory. The advantage of the new resistance pad is that it allows the leg and lever arm to be more closely aligned.
Anatomical Referencing
Anatomical referencing is performed by having the subject actively extend their knee to full extension. The resistance pad is placed in firm contact with the limb while the tester stabilises the distal thigh (a thigh stabilisation strap may be used for this purpose). This active knee extension position is entered a zero degrees. The computer instruction to move the lever arm in a positive direction requires the lever arm and resistance pad, and the subject’s limb, to be moved into flexion.
Gravity Correction
Gravity correction or gravity compensation is performed by then placing the lever arm to an angle corresponding to 45 degrees of knee flexion. This angle could be an angle between 30 and 45 degrees of knee flexion, but should not be ‘as close to the horizontal as possible”. That position would stretch the knee flexors and result in greater resistance than that due to limb segment weights alone. Check that the subject has relaxed the leg and foot by gently moving the foot. Accept the limb weight reading once it is steady.
Range of Movement
For a concentric/eccentric sequence of movement events (muscle actions) for the knee extensors, the stop angle is entered by moving the lever arm, resistance pad and limb to an angle of zero degrees (active full knee extension). The start angle is entered by moving the lever arm, resistance pad and limb to an angle of ninety degrees of knee flexion.
Warm-up
I typically choose to use submaximal efforts to familiarise the subject with the required discrete muscle actions and ensure that the muscle is sufficiently warm to perform maximal efforts. I therefore prefer to use the Start button (which allows discrete efforts) rather than the Warm-up button which allows continuous concentric/eccentric cycles. The usual progression is to ask the subject to produce about 50% of maximal effort in the first muscle actions (concentric and eccentric), then 70 %, then 90%, then 95%, and finally 100%. The eccentric efforts may fall below the requested intensity as they seem more difficult to familiarise the subject with (although the first effort is often strong). Accept the best effort from the screen display until near maximal efforts are produced. Near maximal efforts are required for accurate selection of preload forces.
Pre-loading the Isokinetic Movement
An individualised, not constant, preload is used in all of our strength assessments. This preload may not be optimal, but it should be sufficient to activate the muscle to better than 75% of maximal activation. Achieving an appropriate preload relies on the subject being warm and producing 90 to 95% (of their maximum) effort in their final warm-up efforts. The reason why the preload does not have to be optimal is because we routinely remove the non-isokinetic phases of movement when calculating our measures of strength.
In setting a preload, the aim is to achieve a force (or torque) at the starting angle which is equal to the force (or torque) which would have been achieved had the muscle been maximally activated and moving through the start angle at a constant angular velocity. What this force (or torque) should be may be estimated by extrapolation from the force-angle (or torque-angle) curve produced when the movement is isokinetic (see Kin-Com Isokinetic Knee Testing tutorial). For concentric muscle actions, the preload will be less than that force or torque produced in a maximal isometric muscle action at the specified angle, and will decrease with an increase in the velocity of shortening. For eccentric muscle actions, the preload cannot be greater than that force or torque produced in a maximal isometric muscle action at the specified angle, and so can only be close to that value.
Selecting Maximal Isokinetic Efforts
The overlay screen displayed when using the Evaluation approach to testing shows either the last accepted force-angle curve or an average force-angle curve of all accepted muscle actions. The aim of the testing procedures at each velocity is to obtain the greatest overall force-angle (and hence torque-angle) curve. An example of some representative data is provided below.
Which and How Many Velocities?
As previously stated, our most recent research is investigating the validity of three angular velocities for concentric muscle actions (60, 120 and 180 deg/s) and an angular velocity of 60 deg/s for maximal eccentric muscle actions. We have not incorporated faster eccentric muscle actions because of our concern with the reconstructed joint mechanics and movement through range at faster speeds.
Quantitative Measures of Strength
Data reduction facilities are available after curves have been accepted during the testing phase and the datafile stored. The Numeric and other reports will allow a number of measures of isokinetic strength to be determined. Typically these will include the full range average torque (FRAT), truncated range average torque (TRAT), peak torque (PT), angle specific torque (AST), and work (W). An average power (AP) may also be derived, but this is typically done by using the Kin-Com Analysis Package (KCAP) or by importing an ASCII text copy of the data into a spreadsheet and using a formula to calculate average power. Data can be generated from all torque-angle curves and averaged for each velocity and muscle action, or the best data (highest torque values) may be utilised. In subsequent analyses, ratios such as the torque (peak or average) to body weight ratio, peak torque to average torque ratio, non-dominant to dominant limb ratio, injured to uninjured limb ratio, and/or concentric to eccentric ratio may be derived.
Given the strong correlation between many of these measures of strength, our current practice is to use the truncated range average torque (TRAT) as the measure of strength and to calculate reconstructed to uninjured limb ratios, and concentric to eccentric ratios from the TRAT values.
References
Chapman AJ, Chamberlain VT, Railton RK, Boyle JJW, and Strauss, GR (1995) Extensor strength in the anterior cruciate reconstructed knee. Australian Journal of Physiotherapy, 41(2), 83-88.
Strauss GR, Boyle JJW, and Hopper D. (1996) Knee extensor strength two to four years following ACL reconstruction. A paper presented at the 1996 Annual Conference of the Western Australian Branch of Sports Medicine Australia.
Strauss, G.R., Hickmott, R., Gazis-Morris, A., and Jefferies, S. (1994) Single vs dual pad devices in reducing anterior shear during isokinetic knee extension exercise. Physical Therapy, 74(5), S164. (Abstract)
Strauss, G.R., Boyle, J., Chapman, A., Chamberlain, V., Railton, R., Hickmott, R., Gazis-Morris, A., and Jefferies, S. (1994) Reducing anterior shear during isokinetic knee extension exercise. Book of Extended Abstracts of the 4th International Physiotherapy Congress, pp. 137-139 (Extended Abstract)
[Top]